Atopic Dermatitis
Overview
Atopic dermatitis is one of the more common types of dermatitis. It affects 10 to 30% of children in the United States, with two out of three children affected by the disorder showing symptoms before the age of one, and nine out of ten by the age of five. For half those affected, the disease will go into remission before their teenage years; for the other half, atopic dermatitis will become a lifelong skin condition.
The word "atopy" (from the Greek for placelessness) is used to describe a generalized syndrome of allergic hypersensitivity that tends to run in families. There are several components to the atopic syndrome: along with suffering various manifestations and complications of atopic dermatitis, an individual may also suffer from asthma and/or hay fever.
Symptoms and stages of atopic dermatitis
Symptoms of atopic dermatitis vary widely from person to person, and may even vary from flare-up to flare-up. Infants typically show a red, crusted and oozing rash across much of the body, including the child's legs, feet, hands, arms, face, scalp, and diaper area. In children and adults alike the rash can occur in one or more spots, particularly affecting the upper arms and hands, and creases of the elbows and knees.
The color, size, and intensity of the rash will vary, but the common theme is that it is nearly always itchy, and the itching generally intensifies at night. Those who suffer from atopic dermatitis tend to be more sensitive to the sensation of itching, and scratching can become progressively deeper, longer and more intense. This sets up what is known as the "itch-scratch" cycle, where the more you scratch, the more the rash itches and the more irritated it becomes, thus provoking more scratching.
Along with sleep disturbances, the intense scratching that occurs with atopic dermatitis can lead to additional symptoms and, in some cases, to more serious skin conditions:
- Hyperpigmented eyelids - Inflammation of the skin or hay fever causes the eyelids to become darker in color
- Atopic pleat (Dennie-Morgan fold) - Scratching or rubbing the eyelid causes an extra fold of skin to form under the eyes
- Lichenification - The skin becomes thick and leathery due to the constant scratching
- Papules - These are small raised bumps that can open when scratched causing a crusting of the skin and sometimes infection
- Cheilitis - Skin inflammation on and around the lips
- Ichthyosis - Scaling of the skin that is dry and rectangular in shape
- Urticaria (hives) - Red raised bumps that show up after exposure to an allergen, exercise, or hot bath
- Keratosis pilaris - Rough, small bumps that appear on the upper arms, thighs, and face
- Hyperlinear palms - Increase number and depth of lines in palmar skin
Infants with this skin condition will generally manifest symptoms between 6 to 12 weeks of age. The practice of breastfeeding is associated with a lower incidence in infants. Onset usually affects the face in the area of the cheeks and chin, and looks like a patchy facial rash, which can become red, oozing, and scaling. When an infant starts to crawl, the exposed areas of the knees and elbows may also become affected. By the age of 18 months, many infants demonstrate improvement from atopic dermatitis; however, those affected in childhood may be more vulnerable to dry skin and hand eczema throughout their lives.
Through the tot years and into childhood, the rash changes and appears as papules, which are hard little bumps that become scaly when scratched. The location of the rash typically changes as well, shifting to the inside of elbows, behind the knees, on the sides of the neck, and over the wrists, hands, and ankles. It may also affect the area around the lips and becomes more irritated with licking, which can lead to painful cracking. If the case is severe, it can negatively affect the child's sleep and growth patterns. It is not unusual for children to experience periods of remission that last for months or years. However, the child may experience a reoccurrence during puberty when stress, hormones, and cosmetics can all play a role in flare-ups. It is not unusual for a child who has experienced childhood dermatitis to also experience hay fever and asthma throughout their lifetime.
It is extremely unusual for an adult over the age of 30 to develop atopic dermatitis for the first time, but it's not completely unheard of. Most adulthood cases are individuals who were affected through their childhood years. In adulthood the symptoms do not vary widely from those of childhood. The rash tends to be red, cracked, itchy and dry, and affects mostly the elbow and knee creases, though the hands and feet are also commonly affected. Individuals who are exposed to chemicals or repeated hand-washing are at a far higher risk for a dermatitis flare-up, and workplace-associated dermatitis is a known problem in certain occupations. Atopic dermatitis has also been associated with a variety of ocular complications, such as conjunctivitis and cataracts, so it is a good idea for adult dermatitis patients to have their eyes examined regularly.
Causes of atopic dermatitis
The direct cause of dermatitis is unknown; however, studies have shown that flare-ups are the result of a complex interaction between genetic, emotional, and environmental factors.
Genetically, if member of your family have a history of this skin disease, you too may be predisposed to develop the same skin disease - but this is not a life sentence, since many other factors can be contributory or outweigh a familial predisposition. Emotionally, studies have shown that situations high in stress, anger or frustration can oftentimes trigger an outbreak. Lastly, environmental factors can be broken down into irritants and allergens.
Irritants are substances that are characterized by their direct ability to negatively affect the skin. When skin comes into contact with an irritant in sufficiently high concentration, it will cause the skin to become red, itchy and burning. Depending upon the individual and the irritant, the degree of the rash will vary. Irritants are unique to the individual, and individuals and their families must work together to learn what is causing the skin irritation.
The list of potential irritants is long, but some of the more common irritants are listed below.
- Cigarette smoke can irritate eyelids
- Dust and sand can dry and irritate the skin
- Wool fibers, synthetic fibers, and ill-fitting clothing can rub the skin, triggering the itch-scratch cycle
- Soaps and detergents can dry skin, causing itching to worsen
- Perfumes and cosmetics irritate skin (lanolin from wool can also be problematic)
- Chemicals including chlorine, mineral oil and solvents irritate skin
Allergens are products from foods, animals, or plants that trigger the immune system to overreact, causing an inflammatory response. Allergens are thought to provoke atopic dermatitis through three main points of contact: through direct skin contact, through inhalation, and through ingestion of the allergen. When a person comes into direct contact with an allergen, it triggers inflammation-producing molecules in the body to permeate the skin. This results in the itching and redness associated with dermatitis. When a person with atopic syndrome inhales or ingests an allergen it prompts an over-reaction from the immune system, which in turn triggers skin inflammation, upper respiratory difficulties, and/or gastrointestinal symptoms. These immune-compromising mechanisms can diminish the skin's ability to form new cells and perform its barrier function.
As with irritants, the list of potential allergens is a long one, but here are some of the more common culprits:
- Pollen and pet dander
- Dust mites
- Molds
- Eggs
- Fish
- Dairy products
- Soy products
- Wheat products
Diagnosis and medical treatment of atopic dermatitis
Currently, there is no specific test available to definitively identify atopic dermatitis, mainly because the exact cause remains unknown. A diagnosis is usually made when the doctor and patient work together to compile a complete medical history. Factors taken into consideration when attempting to diagnosis atopic dermatitis include the history of skin rashes experienced by the patient, both in terms of type and locations; the patient's family history of skin rashes and allergies; any allergens and irritants the individual may be in frequent contact with; and an inventory of potential environmental and emotional triggers.
If an allergen is suspected but there is uncertainty, a skin scratch test can be performed to elicit a specific allergenic response. This entails injecting a minute amount of the suspected allergen just beneath the skin's surface, then watching for the skin's reaction. If a red raised bump develops at the site of injection, the individual will know to avoid contact with that specific allergen to prevent any reactions.
Just as there is no clear-cut test for dermatitis, there is also no specific cure for dermatitis, and medical treatment thus focuses on treating symptoms, healing the skin, keeping skin cells healthy, and preventing flare-ups. In minor cases of atopic dermatitis this can be achieved through proper skin care and positive changes in nutrition and lifestyle. In more severe cases a doctor may recommend prescription steroidal creams or oral immune-suppressing medications.
Basic skin care can go a long way toward maintaining optimal skin health and preventing future flare-ups. The simplest thing an individual can do is to make sure the skin is well moisturized. Applying a cream or ointment within three minutes of bathing helps to lock moisture in the skin. Adequate moisture enables the skin to increase its rate of healing as well as establish a barrier against future infection. Most lotions should be avoided due to their high water and alcohol content, which can dry out and irritate the skin. Long hot showers, baths, or dips into hot tubs should be avoided; it's best to limit exposure to 10-15 minutes, and some patients find brief showers or soaks in cool water helpful for breaking the scratch-itch cycle.
Perfumes and cosmetics should also be carefully avoided or limited, as they contain harsh chemicals that can be extremely drying and irritating to the skin. If you use cosmetics, check labels and choose only those that are hypoallergenic, free of fragrances and other toxic or allergenic chemicals.
Over-the-counter topical antihistamines can be helpful for reducing the itching associated with dermatitis. When the itching is stopped, the inflammation and symptoms associated with dermatitis likewise subside.
The following simple lifestyle modifications can make a big difference:
- Identify and avoid contact with anything that can irritate and dry the skin, leading to dermatitis conditions.
- Treat other rashes, e.g., fungal infections, even though they may seem unrelated to the dermatitis.
- Limit scratching, and keep fingernails short to avoid skin abrasions from scratching.
- Use a cold compress to ease the itch and reduce the inflammation.
- Avoid activities that cause sweating and overheating, as they can trigger the start of the scratching cycle.
- Wear loose-fitting cotton clothing, as it tends to feel better against the skin.
- Double-rinse clothing to remove any residual detergent, and always use fragrance-free laundry products.
- Reduce stress, as it is known to be a common cause for dermatitis flare-ups.
Steroidal topical ointments are the most commonly prescribed ointments in the treatment of dermatitis. All but over-the-counter hydrocortisone creams need to be prescribed by your doctor. These creams constrict the blood vessels in the upper dermis of the skin, helping to reduce the itching and inflammation associated with dermatitis.
While steroid creams can be effective in reducing the symptoms of dermatitis, they do not come without side effects. Work closely with your doctor to be fully aware of adverse steroid cream side effects. This will help ensure you derive the most benefit from this type of treatment.
For extreme cases of dermatitis, your doctor may prescribe an oral medication that can suppress the immune system. In more serious cases of dermatitis there is an overactive immune response, and suppressing the immune system can help decrease the symptoms and itching to allow the skin time to regenerate itself and heal.
Alternative treatments for atopic dermatitis
Probiotic, herbal, traditional Chinese medicine and supplemental treatments have all been proven effective in reducing symptoms of atopic dermatitis. Many doctors are familiar with these treatments, as their use is becoming a more common practice in Western medicine.
Probiotics are dietary supplements that contain beneficial organisms such as Lacotobacillus and Bifidobacterium. These bacteria colonize our digestive tracts to help digestion, nutrient uptake, and warding off disease. They also live on our skin. These beneficial flora can be killed off or weakened from overuse of antibiotics, infection, competition from pathogens, poor diet, or other stressors that make our bodies more prone to disease. Supplementing with probiotics aids the body's healing capacity by preserving a healthy balance of good bacteria.
A study done in Australia of 56 children suffering from severe atopic dermatitis showed that taking equal amounts of probiotics, twice daily for a period of eight weeks, reduced dermatitis from severe to mild. Most studies on the effects of probiotics on atopic dermatitis have been performed on children; therefore, it has not been fully established whether adults suffering from atopic dermatitis experience the same positive results.
Many herbalists and homeopathic physicians believe that herbs help cleanse toxins from our system, strengthen our bodies, and allow us to head off skin conditions such as dermatitis. Below are the herbs thought to be most effective.
- Calendula flower, licorice root, and ginkgo all have antiseptic and anti-inflammatory properties. They can be used topically in lotions, oils or ointments applied to the affected area to reduce itching and inflammation.
- Aloe vera gel and the juice and leaves of plantain can be applied topically to the affected areas to help soothe skin irritations associated with dermatitis.
There are also a number of herbal pastes that can be applied topically to help relieve the itching associated with dermatitis.
- Green clay and goldenseal root in equal parts
- Equal parts salt, water, clay, and peppermint oil
- Calamine lotion
- Coal tar lotion, shampoo, and bath oils
Drinking green, black, oolong, and herbal teas can also produce moderate improvement in symptoms. In addition to drinking herbal tea, a chamomile tea bag steeped in hot water, cooled slightly, then placed on the irritated skin can help soothe irritated skin.
Traditional Chinese herbal medicine (TCM) in the form of oral, topical, injectable, and acupuncture treatments has also been found helpful for dermatitis. The three primary functions of TCM are detoxification and elimination, health building, and health management and maintenance. A course of TCM often uses a combination of many different herbs to correct the imbalances in the entire body, not just in the skin.
The first study ever done on Chinese herbal medicine and dermatitis was conducted in London on both children and adults. After given a daily herbal mixture of ten different herbs for two months, the authors found that those taking the herbs had significant improvement of their scaling, redness, inflammation, itching, and other symptoms. Most importantly, they followed up with those patients who continued to use the herbal medicine, and a year later found that their improvements had continued.
As effective as Chinese herbal medicine can be, it's important to note that serious side effects such as liver and kidney toxicity have been linked to treatment in a few case studies. Unfortunately, because of the high variance of herb sources and quality, the exact source of the toxicity was not determined. For best results, consult a qualified practitioner of TCM.
Supplementing your diet with vitamins and minerals has been found safe and effective for improving skin symptoms.
- Vitamin B (B6) plays a role in the metabolism of proteins and fats in our diets, helps counter stress, and maintains a healthy nervous system to benefit dermatitis.
- Folic acid (vitamin B9) levels appear lower in those with dermatitis, and increasing folic acid intake may help improve symptoms.
- Vitamin E and selenium are antioxidants that support metabolic processes and healthy skin.
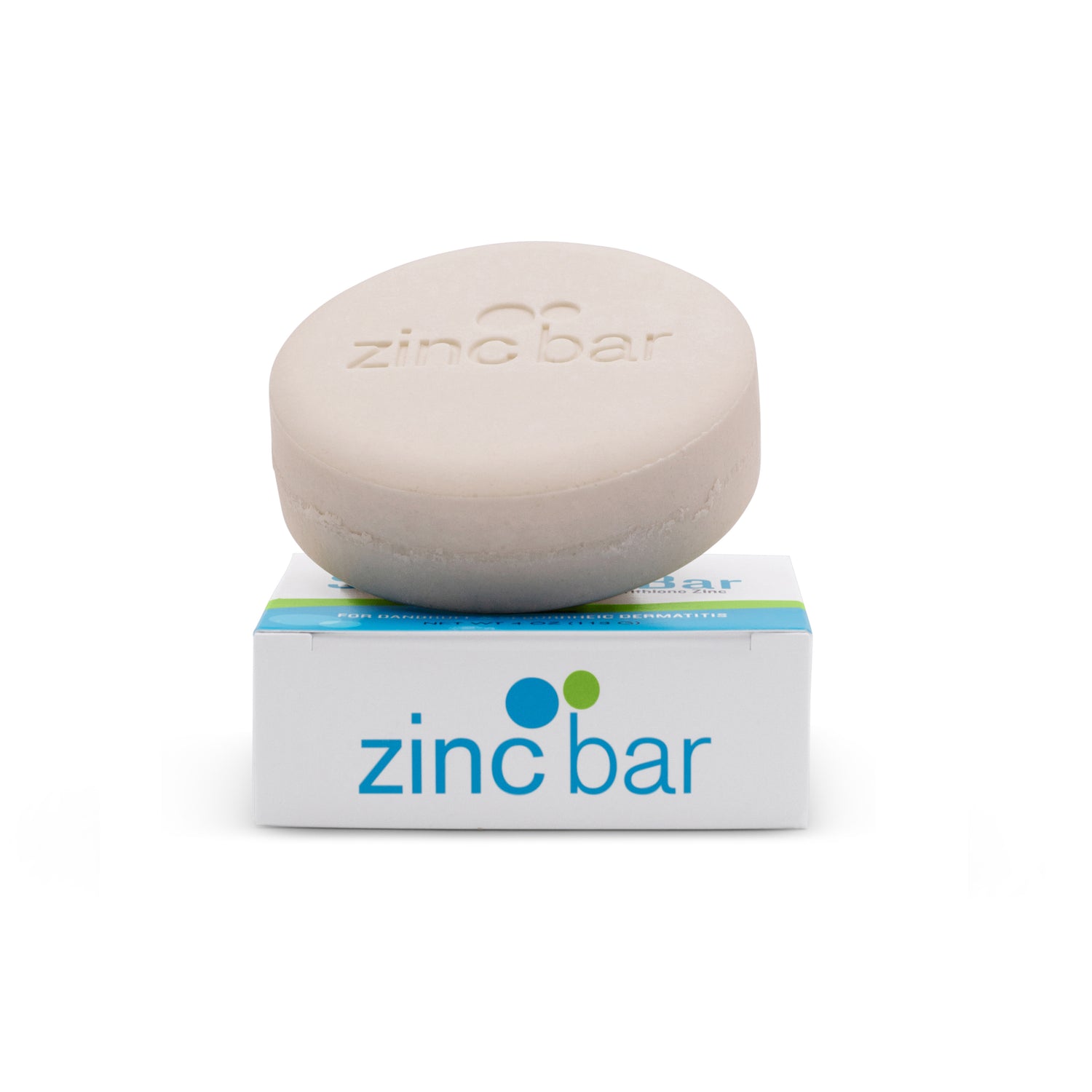
Pyrithione zinc treatment
Pyrithione zinc for centuries has been recognized for its unique healing properties, a number of which have been proven helpful in alleviating dermatitis symptoms.
Pyrithione zinc is an antiseborrheic, which means that it helps to prevent or relieve excessive secretions of the sebaceous glands. These glands lie beneath the skin and work to soften and lubricate the skin and hair. When they become overactive, as occurs during an outbreak of dermatitis, the skin can become inflamed and irritated. Pyrithione zinc's ability to limit seborrheic activity helps reduce the flare-ups of atopic dermatitis.
Pyrithione zinc also has antifungal and antibacterial properties, which may help reduce skin inflammation associated with dermatitis. Topical zinc pyrithione is generally recognized as a safe and effective treatment for reduction in the symptoms associated with certain types of dermatitis.